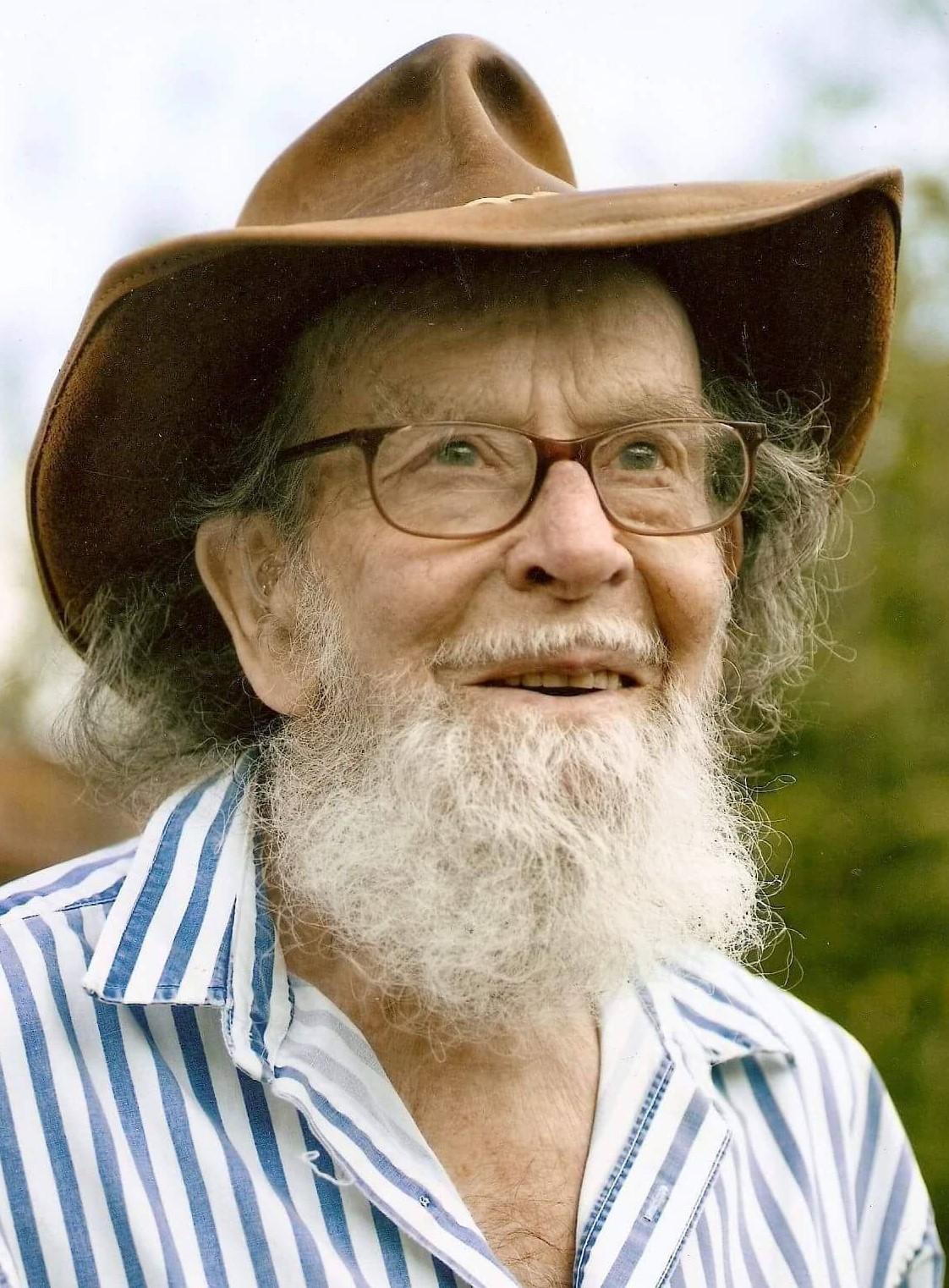
STEPHEN Harrington’s passion in life was horses.
He had his first riding lesson aged five, before galloping off to work in stables as a teenager.
Best known as Alan, the great, great grandfather was a lively character who “would give his last pound to charity”, and was a practical joker known as Andover’s 1st Boys Brigade leader who on camping trips would fill up sleeping bags with cereal or sew them up halfway down.
Alan was one of the first members of the Royal Electric Mechanical Engineers and did an endless list of jobs from being a jockey to a fishmonger, a thatcher, a milkman and more.
He met the love of his life Iris and they married in 1947, going on to have three children together and an open house full of noise, neighbours and friends.
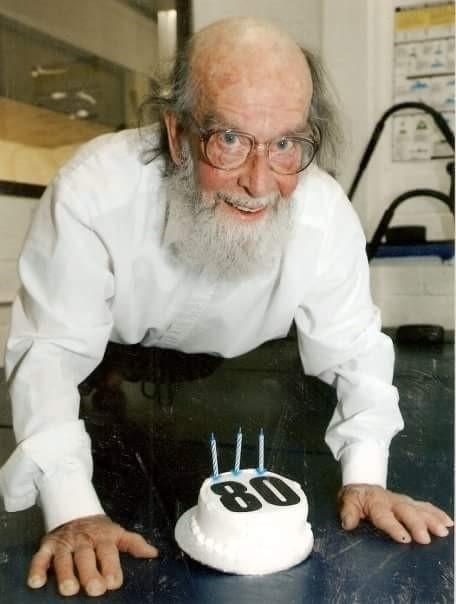
Fast forward to aged 80, and the big kid was doing 80 press ups – with ease – to raise money to rebuild a school in Sierra Leone.
Then, aged 88 in 2010, Alan was diagnosed with dementia.
Daughter Amanda Harrington previously told The Advertiser the struggle that then ensued, as her father’s state deteriorated, to get him into a care home with proper dementia care.
Aged 96 this year, Alan was now paranoid, barricading his door at night, sometimes violent, and living alone in a three-bedroom house, constantly calling the emergency services and Amanda, who received countless voicemails from him crying down the phone.
The family pleaded with Hampshire County Council’s adult social services team to deem him unfit to live alone, and help him move into a care home but, according to its assessments, he had the capacity to live independently, with three care visits a day from government-funded agency Nurseplus.
Amanda, of River Way, said: “They go in and see this person in their home, who perks up because they have got a visitor, and they don’t see how frail and vulnerable they really are and they don’t listen to the families.
“You want to provide the best for your family but you can’t, you can’t do it.
“Nurseplus actually said to them [the council] we have had to take carers out, they can’t give the care he requires.
“That is disgusting for the fact it has been reported to adult social services and they don’t take that into consideration.”
Amanda continued to edge closer to breaking point as her father’s principle carer, being used to three callouts a night to his home while holding down two day jobs.
It was not until August 8 this year, when Alan received skin cancer treatment, that the hospital decided he could not be discharged and go back to his current care package, as it was not deemed suitable.
Alan stayed at Royal Hampshire County Hospital in Winchester for two months and in October the hospital told the family they would look at care homes for him to move into.
But on October 10 in the hospital’s dementia ward, after some eight years since he was first diagnosed with the illness, Alan died.
A day later Amanda received word from the hospital there were no available spaces for him to have moved into a care home in the Andover, Basingstoke or Winchester areas.
Suitable dementia care, Amanda has now also learned, would cost £2,000 a week, and even with the government contributing around £600 a week towards the bill, she has realised her family would not have been able to afford the care their father needed.
Amanda said: “It is a grave situation to be honest.
“In a way I thank God he went into hospital. He got better care, people were with him 24/7.
“I hold adult social services and the government totally responsible, they set the guidelines which are so vastly away from reality.
“We need to press local authorities and government to deal better with this issue.”
For Amanda, key advice for others is to understand the signs of dementia and to try and get a diagnosis made as soon as possible, and put a plan in place.
In response to the family's concerns, Councillor Liz Fairhurst, Hampshire County Council chief for adult social care and health said: “While, we are not able to comment on individual cases, I can confirm that the county council is seeing an increasing number of people living with dementia, who require care, many of whom may live with the condition for some years.
“One of the challenges faced by both those caring for people with dementia, and the person themselves, is the changing nature of the illness, which means that the symptoms and severity may vary from day to day.
“In such situations, we would want to review the support provided to ensure the individual’s varying needs continue to be met.
“This review may include a capacity assessment which is undertaken sensitively – this determines whether an individual is able to make decisions for themselves.
“Ultimately, any person who is able to make and communicate a decision has the right to choose their care, and how they are supported.”
Alan’s celebration of life was held on November 2, on a frosty day with a horse-drawn carriage procession.






Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules here